Group |
Attempts |
Total |
|||||
1 |
2 |
3 |
|||||
n |
% |
n |
% |
n |
% |
||
With borescope |
22 |
91.6 |
1 |
4.2 |
1 |
4.2 |
24 |
Without borescope |
15 |
62.5 |
7 |
29.2 |
2 |
8.3 |
24 |
P: 0.02 (Fisher's exact test) |
|||||||
JSM Clinical Anesthesiology
-
Research ArticleBorescope Vs Laryngoscope in Difficult Airway Management by Non-Expert Personnel: A Non-Randomized Pilot Study in a Simulated EnvironmentValentina Franco Uribe1*, Duván Andrés Vélez Ríos2, Laura Chavarriaga Jiménez3, Juan Diego Pulecio3, Andrés Felipe Prado Reina4, Juan Camilo Gómez Salgado5, and Mauricio Calderón Marulanda51Anesthesiology Resident, CES University, Colombia
2Medical Student, University of Caldas, Colombia
3Medical Doctor, University of Caldas, Colombia
4General Surgery Resident, Military University Nueva Granada, Colombia
5Anesthesiologist, University of Caldas, Colombia*Corresponding author: Valentina Franco Uribe, Anesthesiology Program, CES University, Cl. 10a #22 - 04, Medellin, Antioquia, Colombia, Tel: 573206321211; Email: valenfrancouribe@hotmail.comSubmitted: 07 February 2019; Accepted: 17 April 2019; Published: 19 April 2019 -
Introduction: Though direct laryngoscopy is the method of choice to secure the airway, it has multiple disadvantages. There are different devices to improve the visualization of the airway, but their high cost and need for advanced training limit their use. Borescope would be a cost-effective option with advantages similar to those types of devices.Objective: The primary objective was to compare successful intubation at first attempt with and without the use of borescope. The secondary objective was to compare the average total intubation time with and without the use of borescope.Materials and methods: Controlled non-randomized pilot study in a simulated environment. Population frame work of 48 medical students who received training on the basic management of the device. A difficult airway was recreated in a simulation laboratory using the Laerdal Airway Management Trainer model and intubation parameters were compared using a conventional laryngoscope under direct vision and through borescope.Results: In the group with borescope, 22 out of the 24 participants performed the intubation at the first attempt (91.6%) while in the group without borescope, 15 participants performed the intubation at the first attempt (62.5%) (P: 0.02). No statistically significant difference was found in any other evaluated variable.Conclusion: Borescope could be an effective and economic alternative compared to other devices, since it has similar or better success rates, even for non-expert personnel.Keywords: Airway management; Intratracheal intubation; Equipment and supplies
-
Among the main competences that a general practitioner should have, those related to adequately securing the airway stand out. Failure in achieving adequate airway patency in a patient with difficult airway (DA) may compromise his ventilation and oxygenation. The incidence of DA in surgical population depends on the degree of difficulty; it may range from 1 to 18% in patients who require several intubation attempts [1]. Its incidence in general population varies between 1.15 and 3.8% and failed intubation between 0.13 and 0.3%, which may result in complications as serious as bronchoaspiration, upper airway lesions, cerebral hypoxia, and death [2].Direct laryngoscopy is the method of choice to ensure the airway in both elective and urgent cases. However, multiple disadvantages are observed along this procedure, e.g., difficulty in obtaining optimal glottic visualization or greater cervical spine movement. In the market there are several devices useful to minimize risks, which promise to improve the results and reduce complications. Video laryngoscopes are one of the most used because they obtain higher success rates, but their high cost and the need for a greater learning curve for some of them are the main difficulties that limit their use [3].In this study, a device known as borescope, an optical fiber that allows the visualization of difficult access paths was used. At one end, it has a camera with LED light and, at the other end, an USB connector through which the image is transmitted in real time to a cellular device [4], by means of an Android or IOS application.This pilot test was conducted from September 2017 to March 2018. A call was sent to the medical students of the University of Caldas. To be included the students must have taken and passed the subject ‘anesthesiology and resuscitation’ in the year immediately prior to the study, to be enrolled in the Medicine program, as established in the official curriculum of the University of Caldas. The students were divided into two groups, and they were assigned an odd or even number according to the order of arrival. All participants received instructions on the incorporation of the borescope into the laryngoscope, its basic function and the procedure to be performed. Data collection was carried out in the University’s clinical simulation laboratory using the Laerdal Airway Management Trainer (Laerdal, Stavanger, Norway) for intubation, where a DA was recreated by means of a cervical collar ensuring a Cormack-Lehane III. The USB / borescope device and the Android V3.1 or higher operating system was used, it allowed the USB host on-the-go (OTG) function, through which an interface was established between the device’s camera and the mobile phone to get the image in real time. Cell phones were not specific, however, they all met the criteria requested by the manufacturer of the device, especially, a resolution greater than 640x480 (p/p). In order to properly use the borescope, the “CameraFi” application (Vault Micro Inc., Seoul, Korea) was downloaded for free to each device from the Google Play store (Figure 1).
-
 Figure 1:Borescope attached to the laryngoscope. View Figure
Figure 1:Borescope attached to the laryngoscope. View Figure
The borescope camera was fixed 35 mm from the tip on the base of the Macintosh sheet number 3 with clean adhesive tape (strapper) and its stability was verified; this spot was determined considering that the purpose was to achieve the best visualization with as much anatomical information as possible without missing details in the quality of the image. Each participant performed intubation with orotracheal tube 7.5, with balloon and guide. Once the participant was ready, the timer was set to zero and immediately started when the student took the laryngoscope; the stopwatch was stopped once intubation was declared or after a failure. The intubation of the manikin was verified by insufflation with self-inflating bag (Figures 2 and 3).-
 Figure 2:Use of borescope attached to laryngoscope. View Figure
Figure 2:Use of borescope attached to laryngoscope. View Figure
-
 Figure 3:Management of borescope in the simulation laboratory. View Figure
Figure 3:Management of borescope in the simulation laboratory. View Figure
The primary objective was to compare successful intubation at first attempt with and without the use of borescope. The secondary objective was to compare the average total intubation time until with and without the use of borescope. Evaluated variables: failed intubation, i.e., the impossibility to achieve successful intubation after 120 seconds or after 3 unsuccessful attempts, failed attempt, i.e., when the participant removed the tube from the manikin’s mouth or when esophageal intubation was performed. The number of attempts required by each participant, the total intubation time and whether or not there was esophageal intubation were also evaluated. In addition, 2 subjective variables were recorded: procedure performance difficulty and visualization of vocal cords. The information was collected manually by the research participants and later analyzed with the statistical program Stata version 12. Contingency tables were made, chi test2 and Fisher’s exact tests when there were cells with five cases or less and Student’s t-test for continuous variables with normal distribution.The inclusion criteria stated in this study were met by 48 students; all the participants were included in the final analysis. There were 2 failed intubation cases in the group without borescope (8.3%) and one case in the group with borescope (4.2%). However, this difference is not statistically significant (P: 0.5). In the group with borescope, 22 out of the 24 participants performed the intubation at the first attempt (91.6%), compared with 15, out of 24 (62.5%), in the group without borescope (P: 0.02). The variable number of attempts is also affected by the use of borescope since most participants who used it required one attempt to achieve successful intubation, while a greater proportion of participants who did not use borescope required more attempts (Table 1).-
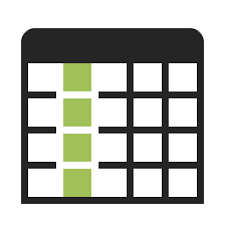 Table 1:Number of intubation attempts according to group. View Table
Table 1:Number of intubation attempts according to group. View Table
No statistically significant differences were found in the average total intubation time (40.09 ± 5.85 in the group without borescope and 45.42 ± 6.39 in the group with borescope; Student t-test P: 0.5). Although a trend towards greater number of esophageal intubation was found (2 cases in the group without borescope (8.3%) and none in the group with borescope), it was not statistically significant (P: 0.2). Similarly, no differences were found in the number of students who reported difficulty during the procedure (29.2% without borescope and 37.5% with borescope, P: 0.3). However, a higher proportion of students who used borescope reported having visualized the glottis (87.5%), compared with the group without borescope (62.5%), P: 0.04.This pilot test confirmed that borescope could be an effective alternative to improve the success rate of orotracheal intubation at the first attempt, even in non-expert personnel. A 2016 Cochrane systematic review included 64 studies with 7044 adult participants and compared the use of video laryngoscope (VL) of one or more designs with a Macintosh laryngoscope [5]. The authors concluded that VL may reduce the number of failed intubations, particularly among patients who have a difficult airway, improve glottic vision and decrease laryngeal trauma. There is no difference in patients with airway defined as normal or without predictors of difficult airway; this due to the great heterogeneity in the results dealing with time, attempts and failures in intubation. This is why the borescope model recreating a DA was used; the main finding was that, with the device, the rate of successful intubations in the first attempt (91.6%) increases significantly with respect to the exclusive use of laryngoscope (62.5%).The first attempt to manage a borescope is not easy for students; it requires a greater learning curve. However, due to the number of successful intubations at the first attempt and the greater visualization of the glottis, it could be easily handled by non-expert personnel. Borescope use may be a part of training and teaching in medical students, by clinical simulation in different scenarios to improve psychomotor skills and abilities in anesthesia practice [6], mainly in airway management.There is a growing implementation of technology in the practice of anesthesiology and related areas. Sheraton et al. [7], described the use of smart phones for development in the world of anesthesia and the success they will have in clinical practice. The different applications in smart phones are available for free, like the application used in this study, which guarantees easy access for borescope use, thus, success is expected. Low D and Groos [8] used an IOS device to assist nasal fiber optic intubation in a simulation model and improved intubation times in all attempts. These findings are important since they give rise to different management alternatives in different areas of anesthesiology and resuscitation in a world that technologically advances very fast; they also open the way to other works of research about borescope, and not exclusively in airway management.We found very few studies about the use of this device in humans. Ahmad Sabry et al. [9], used borescope for nasal intubation and concluded that it would be an economical alternative to a fibrolaryngoscope since they used it with 8 patients without any complications. Karippacheril et al. [10], reported their initial experience with the device in 24 patients older than 16 years taken to elective surgery; these researchers intubated 22 patients at the first attempt, and the other 2 required 2 attempts, none of them had associated complications. The authors concluded that this is a personal and economic device and that it is safe and reliable for clinical use.Additionally, Chaparro et al. [2], conducted a non-systematic review to show the current state of videolaryngoscopes and their impact on airway management. The authors argue that the visualization of the larynx through devices such as VL does not guarantee the success of intubation, that the effectiveness of VL in AD has limited evidence and that the success of intubation with VL is related to experience in its management, with a learning curve that does not exceed 10 patients. Finally, the authors conclude that there are still controversies in the management of AD and the safety it represents for patients. Considering these aspects, it is important to conduct future research regarding the limitations that borescope could have both in airway management and in its safety, which will require different studies despite the fact that it has been shown to be safe in humans.It would be necessary to conduct controlled clinical trials in simulation scenarios and later with actual patients in order to compare the use of borescope with other devices, such as videolaryngoscopy and standard laryngoscope.Although borescope is a new device and it has not been proven as a clinical tool in airway management, it could work as an effective and cheaper alternative to other devices with similar or even better successful rates.Dr. Fernando Arango, for his collaboration in the design and analysis of this studyFinancingThe funds used for this pilot study were provided by the researchers. No financial assistance was received from any other institution and / or person outside of it. The University of Caldas provided the clinical simulation laboratory where the model Laerdal Airway Management Trainer (Laerdal, Stavanger, Norway) was used for intubation, and other equipment. There were 4 borescopes which were acquired with the researchers’ own resources for an approximate price of 10 US dollars each.LimitationsVery few studies that could serve as a reference have used borescope as a clinical tool in patients as well as in simulation scenarios. This pilot test is limited because the students were not assigned randomly to the use of the borescope and also due to small sample size given the difficulty of finding students that met the inclusion criteria. -
-
- Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991; 75: 1087-1110.
- Chaparro-Mendoza A, Luna-Montúfar CA, Gómez JM. Videolaryngoscopes: the solution for difficult airway management or just another strategy? Systematic review. Rev Colomb Anestesiol. 2015; 43: 225-233.
- Karippacheril JG, Le Cong M. Videolaryngoscopy using an Android smartphone: a direct digital technique. Indian J Anaesth. 2016; 60: 143-145.
- Trivedi JN. An economical model for mastering the art of intubation with different video laryngoscopes. Indian J Anaesth. 2014; 58: 394-6396.
- Lewis S, Nicholson A, Cook T, Smith A. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation for general anesthesia. Cochrane Database Syst Rev. 2016; 11: CD011136.
- Gómez LM, Calderón M, Sáenz X, Reyes G, Moreno MI, et al. Impact and benefit of clinical simulation in the development of psychomotor skills in anesthesia: a double blind randomized clinical trial. Rev Col Anestesiol. 2008; 36: 93-107.
- Sheraton TE, Wilkes AR, Hall JE. Mobile phones and the developing world. Anaesthesia. 2012; 67: 945-950.
- Low D, Goos M. Using an Apple iPad to assist fibreoptic intubation. Anaesthesia. 2012; 68: 110-111.
- Ahmad Sabry MHI, Aboughazy A. The use of Usb endoscope (borescope) to guide nasal intubation - a pilot study. Abstract PR528. Anesth Analg. 2016; 123: 237.
- Karippacheril JG, Umesh G, Ramkumar VJ. Inexpensive videolaryngoscopy guided intubation using a personal computer: initial experience of a novel technique. Clin MonitComput. 2014; 28: 261.