|
|
No. |
% |
Age |
Range |
37-79 |
|
Mean±SD |
60.93±9.18 |
||
Sex |
Female |
3 |
6.7 |
Male |
42 |
93.3 |
|
Performance and co-morbidities |
|||
Performance Status |
Ps 0 |
1 |
2.2 |
Ps 1 |
27 |
60 |
|
Ps 2 |
17 |
37.8 |
|
Hypertension |
Yes |
9 |
20 |
Piles |
Present |
12 |
26.7 |
Previous Bilharzial infestation |
Yes |
33 |
73.3 |
Diabetic |
Yes |
4 |
8.9 |
Smoking |
Smoker |
32 |
71.1 |
Presenting symptom |
|||
Hematuria |
No |
11 |
24.4 |
Initial |
10 |
22.2 |
|
Terminal |
7 |
15.6 |
|
Cystitis |
Yes |
45 |
100 |
Urgency |
Yes |
18 |
40 |
Retention |
Yes |
1 |
2.2 |
Pain |
Yes |
31 |
68.9 |
Urinary tract infection |
Pus cells |
11 |
24.4 |
Tumor characteristics |
|||
Tumor site |
Anterior |
3 |
6.7 |
Posterior |
9 |
20 |
|
Lateral |
7 |
15.6 |
|
Antero-lateral |
7 |
15.6 |
|
Postro-lateral |
8 |
17.8 |
|
Vault |
3 |
6.7 |
|
Ureteric orifices |
2 |
4.4 |
|
Bladder neck |
1 |
2.2 |
|
Multi-centeric |
5 |
11.1 |
|
Tumor gross pattern |
Endophytic |
1 |
2.2 |
Exophytic |
44 |
97.8 |
|
Histopathology |
TCC |
34 |
75.6 |
squamous differentiation |
11 |
24.6 |
|
Hydronephrosis |
Yes |
13 |
28.9 |
T stage |
T1 |
1 |
2.2 |
T2 |
26 |
57.8 |
|
T3 |
18 |
40 |
|
N stage |
N0 |
45 |
100 |
Grade |
G2 |
11 |
24.4 |
G3 |
34 |
75.6 |
|
Stage |
I |
1 |
2.2 |
II |
26 |
53.3 |
|
III |
18 |
44.4 |
|
Complete TURBT |
Yes |
34 |
75.6 |
JSM Radiology and Radiation Therapy
-
Review ArticleGemcitabine Based Hypofractionated Chemoradiation in Treatment of Muscle Invasive Bladder CarcinomaAbdelmalik NA¹*, Tareq salah², and Diaa Hameed³1Department of Radiotherapy and Nuclear Medicine, Assiut University, Egypt
2Department of Clinical oncology, Assuit University, Egypt
3Urology department, Assuit University, Egypt*Corresponding author: Noha Ali Abdelmalik, MD, Lecturer of Radiation oncology, SECI, Assuit University, Egypt, Email: noha_soli_2010@yahoo.comSubmitted: 19 February 2019; Accepted: 19 April 2019; Published: 22 April 2019 -
Introduction: Bladder cancer is a global health problem worldwide and the ninth most common cancer. The most appropriate treatment algorithm for muscle-invading disease remains controversial. Although radical cystectomy has been the mainstay for treatment for decades, organ preserving regimens using predominantly multiple modality therapy are emerging as viable proven alternatives in a subset of patients. The RTOG 95-06 study, examining the combination of hypo fractionation with chemotherapy, showed a 67% complete response rate and a 3-year survival rate of 83 %.Objectives: This prospective study aimed at evaluation the efficacy and toxicity of a modified hypo fractionated chemo radiotherapy protocol for patients with muscle invasive bladder cancer.Patient and methods: This prospective study was conducted during the period from April 2012 to end of 2016 in the radiotherapy department, South Egypt Cancer Institute, clinical oncology department, Assiut University Hospital and urology hospital Assiut University. Forty-five patients, 37-79 years old, transitional cell carcinoma, stage 57.8% T2, 40%T3, N0, M0 after transurethral resection [24.4% complete TUR and 75.6% incomplete TUR] and magnetic resonance imaging, were recruited. Patients were treated with hypo fractionated radiotherapy [RT] schedule that delivered 52.5 Gy in 20 fractions with weekly Gemcitabine 100mg/m².Results: The majority of patients achieved complete response (CR) up to 86.7% and 13.3% with partial response. Three patients only (6.7%) suffered from G3 acute bladder toxicity but no G3 proctitis. The 2-year overall survival [OS] rate recorded 93.3%and progression free survival [PFS] (82.8%)in favor of hypofractinated radiation schedule regarding standard conventional one. The multivariate analysis showed TUR as the only factor affecting OS [0.002] and PFS [0.38] significantly.Conclusion: The hypo fractionated radiation proved to be of higher CR rate and survival rate with the favorable toxicity profile than that of conventionally fractionated radiation schedule given concurrently with Gemcitabine. Also, the schedule is tolerable and cost effective as well.
-
Bladder cancer represents a health problem worldwide as it is the ninth common cancer in both males & females. It is the most common malignant disease involving the urinary system and the second most common genitourinary cancer. Bladder cancer accounts for approximately two-thirds of all urinary tract cancers in United States. The estimated annual incidence in the United States of 68,810 cases, accounting for 5% of all newly diagnosed cancers. In Egypt, the situation of bladder cancer is very special. It has been the most frequent malignancy among male. Liver and bladder cancers represented approximately 44% of cancer in males. Bladder cancer ranked next to liver cancer in Lower Egypt (8. 8%).In Upper Egypt, liver cancer was still the most common cancer, with a small difference from bladder cancer (12.6%). Bladder cancer ranked second in males [1,2].The main risk factor for bladder cancer in Egypt was urinary Schistosomiasis which was more frequent in Upper Egypt and its prevalence decreased when going north. The age-standardized rates are 16.9/100,000 (more developed) and 5.3/100,000 (less developed) compared to 21.1/100,000 in Egypt [2].Primary cystectomy is considered the main treatment but, it carries significant physical, sexual, psychological morbidity. Also, quality of life can be impaired, even with neobladder reconstruction [3]. Therefore, increasing interest in using bladder preservation approaches in selected patients, which provide equivalent tumor control and to minimize treatment-related morbidity [4].Maximal transurethral resection of bladder tumor (TURBT) followed by irradiation with concurrent chemotherapy has emerged as viable proven alternatives in a subset of patients. Refining the treatment choice by maximizing the quality of life without compromising survival rates is the goal [3]. Combined modality therapy achieves a CR and preserves the native bladder in roughly two-thirds of patients, while offering long-term survival rates comparable to contemporary radical cystectomy series for patients of similar clinical stage. Altered radiotherapy fractionation has been intensely investigated during the past 20 years. A reduction of the overall treatment time (acceleration) has shown some improvement in radiotherapy efficacy in headand- neck and lung cancer [4]. The effectively applied high dose radiotherapy fractions have been in clinical practice with 5-year local control rates of 20% to 30%. The RTOG 95-06 study, showed a 67% complete response rate and a 3-year survival rate of 83 %in the combination of hypo fractionation with chemotherapy [5].This study is the first study to be conducted in our locality to revise these data in our patients as this beside added clinical benefit may help to decrease the overload on our fully loaded radiotherapy machines hoping to shorten waiting lists.This single arm, phase II prospective study was conducted during the period from April 2012 to end of 2016 in the radiotherapy department, South Egypt Cancer Institute, clinical oncology department, Assiut University Hospital, Assiut University and urology hospital, faculty of medicine, Assiut University. Informed consent was obtained from all recruited patients with Institutional Review Board approval for the protocol. Patients with cT1-3, N0, M0 bladder cancer who underwent maximum TURBT were eligible for the study. Baseline evaluation of each patient included chest radiograph, abdomen-pelvic magnetic resonance imaging (MRI)/computed tomography (CT), bone scan (if ≥T3 , bone pain or elevated alkaline phosphatase), full blood picture, kidney and liver function tests, performance status ≤ 2 according to ECOG scoring system , hemoglobin ≥ 10 mg/dl, an absolute neutrophil count of ≥1500/ml, a platelet count of > 100,000/mm3, a serum creatinine of 1.5 mg% or less, a serum bilirubin less than or equal to 1.3 time of Upper limit of normal, were included in current study. Patients with previous pelvic radiation therapy, patients with node positive disease, evidence of distant metastasis (M1) were excluded from study. All patients in this study underwent maximum transurethral resection of bladder cancer.Radiotherapy planningAll patients were planned through CT simulator-based planning with isocentric technique. Patients received hypo fractionated radiation schedule in form of 5250 cGy/20 fractions by 262.5 cGy per fraction, over 4 weeks with weekly concurrent gemcitabine 100 mg/m2. Clinical target volume (CTV) had included the whole bladder + 1.5cm margins all around.Assessment of response to treatmentResponse to treatment was evaluated 3 months after completion of treatment by MRI scans of the abdomen and pelvis together with cystoscopy under general anesthesia with biopsy from any suspicious lesion. Additional cystoscopy was performed at 7 and 12 months and every 6 months thereafter. Repeat MRI scans were undertaken at 12 months and 24 months. Complete response was defined as the absence of visible tumor endoscopically and the absence of histologic evidence of disease.Acute treatment related toxicity was assessed weekly during treatment and on the final day of treatment. After completion of treatment, acute toxicity was scored for additional 6 weeks and it was expressed by using the RTOG/EORTC Radiation Toxicity Grading.Late treatment related toxicity was assessed monthly up to one year starting from 6 weeks from end of chemoradiation course and then every 6 months with time of cystoscopy and imaging evaluation. Patients were assessed based on RTOG/ EORTC Radiation Toxicity Grading.Treatment InterruptionIf any grade 3 hematological toxicity develops, chemo radiotherapy should be discontinued for one week. For a grade 3 in field (radiation-related) toxicity during any treatment week (such as radiation cystitis, acute colitis), chemotherapy and radiation therapy should be delayed until resolution of toxicity to grade 2 or less. If the delay to resume treatment is greater than three weeks, the patient should be considered intolerant to protocol therapy and considered off-protocol and will be referred to radical cystectomy.Statistical analysisOverall survival was defined as the time from diagnosis till death or last follow up visit at time of analysis.Progression free survival was defined as the time from diagnosis till time of clinical, radiological progression OR death.Patient characteristicThe mean age of patients was 58 years (range 37 - 79 years), 93% (42 patients) were males. History of bilharzial infestation was noted in 73.3 % (n=33) of patients. Three quarters (34 patients) presented with hematuria (75%). T staging showed that 2%, 58%, and 40%of patients presented with T1, T2andT3 disease respectively. The majority of patients (75.6%) presented with high grade tumors (34 patients).All patients underwent maximal TURBT, but complete TUR was achieved in 34 % of patients. Pathological report documented pure TCC in 76% (n=34), transitional cell carcinoma with squamous differentiation was noted in 11 patients (24%) (Table 1).
-
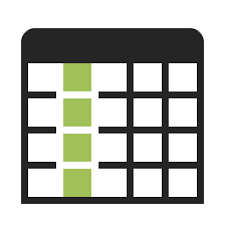 Table 1: Patients’ characteristics. View Table
Table 1: Patients’ characteristics. View Table
Treatment outcome39 patients (86.7%) had CR, and 6 patients had partial response (PR); of them 3 patients showed muscle invasive bladder cancer (MIBC) and were shifted to radical cystectomy, 2 patients had non MIBC and shifted to intravesical instillation of BCG (Figure 1). Only one patient has progressed and discovered to have bone metastasis at the end of chemoradiation (Table 2). Median progression free survival was 12 months (Figure 2) and median overall survival was 18 months (Figure 3).-
 Figure 1: Kaplan Meier curve showing significant influence of TUR on OS. View Figure
Figure 1: Kaplan Meier curve showing significant influence of TUR on OS. View Figure
-
 Table 2: Results. View Table
Table 2: Results. View Table
-
 Table 3: Univariate analysis of factors that might influence OS and PFS. View Table
Table 3: Univariate analysis of factors that might influence OS and PFS. View Table
ToxicityHypo fractionation chemoradiation protocol was well tolerated for majority of patients with mild to moderate complains, that improved with supportive medical treatment. Three patients (6.7%) had suffered from G3 cystitis, 67% (30 patients) developed G2 cystitis, and 15% (7 patients) had enteritis. During follow up, only one patient was reported changes in bladder capacity with increased frequency of micturition. All symptomatic patients responded to medical treatment and completed the full planned course of chemoradiation.Survival ratesAfter time of analysis, Table (3). Univariate analysis of factors that might influence OS and PFS in patients showed that TUR adequacy was the only factor that affected OS (P =0.001) (Figure 1).Hypo fractionated radiation therapy can provide many advantages to both cancer patients and health care providers (radiotherapy departments). It could be considered as possible alternative to conventional radiotherapy schedules. Two published UK-based randomized controlled trials allowed the use of conventional (6400 cGy/ 32 fr.) and Hypo fractionated Radiotherapy (5250 cGy / 20 fr.)[10,11]. Neither study showed difference in outcome based on dose and fractionation. Many reported studies showed favorable treatment outcome and tolerable toxicity profiles of hypofractionated radiotherapy protocols [6,7,8,9,10]. Analysis of our study showed high response rate with 86.7% (n=39) complete response and 4.4% (2 patients) have got partial response with non-muscle invasive disease so treated conservative maneuver. The OS in hypofractionated radiation protocol was 93.3% which is comparable OS to that documented in conventional chemoradiation protocols of bladder cancer management. These results are confirmed by previously published series including phase II study of conformal hypofractionated radiotherapy with gemcitabine in which 88% of patients achieved complete response, 3-year overall survival was 75% and disease specific survival was 82% [11]. Another published study by Christe group who had studied hypofractinated radiotherapy alone in treatment of 60 selected patients, had demonstrated 75% complete response rate and 61% overall survival [7]. Radiation Therapy Oncology Group 95-06 had studied combination of hypofractionation with cisplatin and showed 67% complete response rate, 3-year survival rate 83% [5]. Regarding to the factors affecting outcome, current study analysis showed that complete TURBT is the only significant factor affecting overall survival (P=0.001) with a trend towards improving relapse free survival (0.06) (Table 3). Median progression free survival was 12 months (Figure 2) and median overall survival was 18 months (Figure 3).-
 Figure 2: Median Progression free survival. View Figure
Figure 2: Median Progression free survival. View Figure
-
 Figure 3: Median Overall Survival. View Figure
Figure 3: Median Overall Survival. View Figure
As early toxicity is considered dose limiting in altered fractionation radiotherapy, conformal radiotherapy emerged as bright way to spare early reacting normal tissue. Bowel sparing technique would not only reduce treatment toxicity, but also would enhance the surgeon’s ability to create continent diversions after pelvic radiation if salvage surgery was needed. It was approved in studying patients with bladder cancer used concomitant boost technique with small pelvic field was planned to increase dose to bladder gross. That technique reduced acute bowel toxicity (G2) to 14% but had similar response to conventional dose series [12]. So, to irradiate bladder only with margins as modeling study documented that the choice of margins was as important as the choice of fractionation in term of intestine, rectum dose volume histogram data and normal tissue control probability predictions [13]. Our study can confirm that bladder only radiation is as effective as pelvic radiation in disease relapse survival. Similar results were published by single institutional study that compared bladder only concurrent chemoradiation (BO-CCRT) vs. whole pelvis (WP-CCRT) in lymph node negative invasive bladder cancer. In reported study, WP-CCRT was associated with a 5-year disease-free survival of 47.1% compared with 46.9% in patients treated with BO-CCRT. The bladder preservation rates were 58.9%and 57.1% in WP-CCRT and BO-CCRT, respectively and the 5-year overall survival rates were 52.9% for WP-CCRT and 51% for BO-CCRT (p= 0.8). In WPCCRT group, 42.9% had regional lymphadenopathy recurrence [15]. German study of a combined modality treatment for locally advanced bladder cancer 415patients with bladder cancer (high-risk T1or T2-4) received radiotherapy or chemoradiotherapy after TURBT. A CR was achieved in 72% of the patients. The 10-year disease-specific survival rate was 42%, and more than80% of survivors had their bladder preserved [16]. Our study showed comparable bladder preservation rate 77.8%. Patients in hypofractionated schedule had no significant changes in sexual function and associated with statistically significant less acute bladder toxicity and small bowel toxicity (G2). Only3 patients (6.7%) have experienced radiation cystitis G3. Hematologic toxicity was minimal. Our study can demonstrate significant benefit of hypofractionation schedule in bladder cancer management and better toxicity profile than conventional chemoradiation schedule. -
-
- Avritscher EB, Cooksley CD, Grossman HB, Sabichi AL, Hamblin L, Dinney CP, et al. Clinical model of lifetime cost of treating bladder cancer and associated complications. Urology. 2006; 68: 549-553.
- Sami AI, Mikhail NNH et al. Egypt National Cancer Registry, Damietta Profile, Publication Number RR2. 2011; 67-71.
- Jason A, Efstathiou, Anthony L, Zietman, et al. Clinical radiation oncology, 3rd Edn. Bladder Cancer, 2012; 52: 1099-1123.
- Zouhair A, Ozsahin M, Schneider D, Bauer J, Jichlinski P, Roth A, et al. Invasive bladder carcinoma: a pilot study of conservative treatment with accelerated Radiotherapy and concomitant cisplatin. Int J Cancer. 2001; 96: 350-355.
- Kaufman DS, Winter KA, Shipley WU, Heney NM, Chetner MP, Souhami L, et al. The initial results in muscle invading bladder cancer of RTOG 95-06: PhaseI-II trial of transurethral surgery plus radiation therapy with concurrent cisplatin and 5-fluorouracil followed by selective preservation or cystectomy depending on the initial response. Oncologist. 2000; 5: 471-476.
- Michael I. Koukourakis, Christos Tsolos, and Stavros Touloupidis; Radical Hypo-fractionated Accelerated Radiotherapy with Cytoprotection for Invasive Bladder Cancer. Urology. 2007; 69: 245-250.
- Kaufman DS, Winter KA, Shipley WU, Heney NM, Chetner MP, Souhami L, et al. The initial results in muscle-invading bladder cancer of RTOG 95-06: Phase I-II trial of transurethral surgery plus radiation therapy with concurrent cisplatin and 5-fluorouracil followed by selective preservation or cystectomy depending on the initial response. Oncologist. 2000; 5: 471-476.
- Pos FJ,Hart G, Schneider C, Sminia P. Radical radiotherapy for invasive bladder cancer: What dose and fractionation schedule to choose?. Int J Radiat Oncol Biol Phys. 2006; 64: 1168-1173.
- Mutahir A. Tunio MA, Hashmi A, Qayyum A, Mohsin R, Zaeem A. Whole-pelvis or bladder-only chemoradiation for lymph nodenegative invasive bladder cancer: single-institution experience. Int J Radiat Oncol Biol Phys. 2012; 82: 457-462.
- Sangar VK, McBain CA, Lyons J, Ramani VA, Logue JP, Wylie JP. Phase I study of conformal radiotherapy with concurrent gemcitabine in locally advanced bladder cancer. Int J Radiat Oncol Biol Phys. 2005; 61: 420-425.
- Borut K, Lijana ZK. Phase I study of radiochemotherapy with gemcitabine in invasive bladder cancer. Radiother Oncol. 2012; 102: 412-415.
- Oh KS, Soto DE, Smith DC, Montie JE, Lee CT, Sandler HM. Combinedmodality therapy with gemcitabine and radiation therapy as a bladder preservation strategy: long term results of a phase I trial. Int J Radiat Oncol Biol Phys. 2009; 74: 511-517.
- Choudhury A, Swindell R, Logue JP, Elliott PA, Livsey JE, Wise M, et al. Phase II Study of Conformal Hypofractionated Radiotherapy with Concurrent Gemcitabine in Muscle-Invasive Bladder Cancer. J Clin Oncol. 2011; 20: 733-738.
- Cowan RA, McBain CA, Ryder WD, Wylie JP, Logue JP, Turner SL, et al. Radiotherapy for muscle invasive carcinoma of the bladder; results of a randomized trial comparing conventional whole bladder with doseescalated partial Bladder radiotherapy. Int J Radiat Oncol Biol Phys. 2004; 59: 197-207.
- Tunio MA, Hashmi A, Qayyum A, Mohsin R, Zaeem A. Whole-pelvis or bladder-only chemoradiation for lymph node-negative invasive bladder cancer: single-institution experience. Int J Radiat Oncol Biol Phys. 2012; 82: 457-462.
- Rödel C, Grabenbauer GG, Kühn R, Papadopoulos T, Dunst J, Meyer M, et al. Combined-modality treatment and selective organ preservation in invasive bladder cancer: long-term results. J Clin Oncol. 2002; 20: 3061-3071.