Unprecedented Brain Imaging Findings in a Case of Acute Disseminated Encephalomyelitis
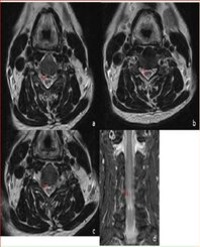
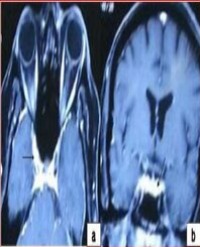
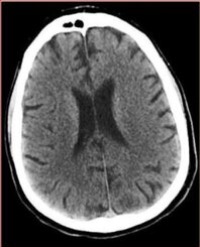
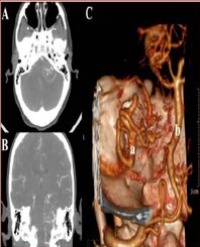
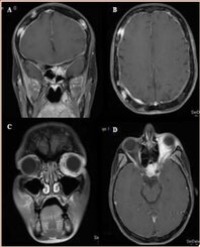
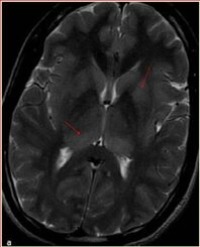
Acute Disseminated Encephalomyelitis (ADEM) is an acute widespread autoimmune demyelinating disease affecting central nervous system. It is characterized by multifocal white matter lesions on neuroimaging. Grey matter can also be affected, particularly basal ganglia, thalami, and brainstem. Variant Creutzfeldt - Jakob disease (vCJD) is a rare and fatal human neurodegenerative condition affecting younger patients. Pulvinar sign on Magnetic Resonance Imaging (MRI) is considered to be a strong indicator of variant CJD. We report a young patient who presented with febrile illness and altered mental state. Brain imaging revealed hyperintensity in bilateral medial and posterior thalamus. These imaging abnormalities are similar to those seen in variant CJD.
Mahale R¹, Mehta A¹, and Rangasetty S¹*